Psychosocial Assessment and Related Factors for Kidney Transplantation Candidates in South Korea: A Descriptive Correlational Study
한국 신장이식 대기자의 심리사회적 평가 및 영향 요인
Article information
Abstract
Purpose: The purpose of this study was to assess the psychosocial status of candidates for deceased donor kidney transplantation (DDKT) in South Korea and identify factors associated with high-risk psychosocial status. Methods: The descriptive cross-sectional design included application of a standardized transplantation-specific assessment tool, the Psychosocial Assessment Candidacy Transplantation (PACT) instrument, and review of candidates’ medical records. A total of 157 patients awaiting DDKT were recruited from a Korean organ transplantation center. The collected data were analyzed using descriptive statistics and binary logistic regression. Candidates were divided into high- and low-psychosocial risk groups using 3 as the cutoff point of PACT. Results: The mean score for the PACT final rating was 2.10, and the lowest average subscale score was 2.30 for understanding the processes of transplantation and follow up. Poor physical candidacy, especially due to comorbidities, and older age were associated with high psychosocial risk. Conclusion: The results of this study showed that the psychosocial status of Korean DDKT candidates was problematic. Development of systematic management programs for effective clinical strategies in the care of candidates is crucial to maintain their desirable psychosocial status in case of an emergency DDKT operation and improve post-transplantation outcomes. Continuous education is absolutely necessary to enhance understanding of the transplantation process for high-risk psychosocial candidates. Additionally, nurses and transplantation professionals should screen candidates with high-risk psychosocial status early in the process using transplantation-specific assessment tools and provide intensive interventions, particularly for poor physical candidacy patients and older candidates.
INTRODUCTION
1. Background
The number of people diagnosed with end-stage renal disease (ESRD) is increasing as a result of the aging society in South Korea and a corresponding increase in chronic disease [1]. Kidney transplantation (KT) is known to be the best treatment option for people with ESRD; it can improve quality of life, alleviate suffering from uremic symptoms, and offer a chance to live longer when compared to dialysis [2-4]. For these reasons, ESRD patients are more likely to choose transplantation over dialysis, and the number of candidates for deceased donor kidney transplantation (DDKT) has steadily increased with 21,048 patients on the KT waiting list in 2018 [5].
However, the deceased organ donation rate in Korea is nine per million people annually, which is only one-quarter to one-fifth that in countries such as Spain (47 per million) and the United States (32 per million) [5]. Furthermore, since 2016, the annual number of organ donations in Korea has been decreasing due to several social issues. For example, negative media reports on donor families’ dissatisfaction with how they were treated after organ donation—such as receiving little or no support and respect from medical personnel during the funeral process—have created negative perceptions about organ donation among the public. In addition, the families of some end-stage patients who are potential organ donors decide to withdraw them from life-sustaining treatment, which deprives them of the chance to donate their organs [6]. From the hospital perspective, labor shortage, due to the enforcement of a statutory working hour limitation for healthcare workers, has created donor management issues [6]. Therefore, the discrepancy between the number of patients awaiting KT and the deceased donor kidney supply is rapidly growing larger. These and other factors create a serious problem for those awaiting transplants and compared with ESRD patients in many Western countries, Koreans are experiencing a longer waiting time for DDKT. In fact, according to the annual report of the Korean Network for Organ Sharing (KONOS) [5], the mean waiting time for DDKT increased from 1,732 days in 2012 to 1,955 days in 2017. Additionally, DDKT candidates are faced with longer waiting times than candidates for other organ transplants.
The prolonged waiting times result in physical and psychosocial issues for DDKT candidates. The literature shows that compared with the general population, candidates on the waiting list for DDKT have higher mortality rates, more complex medical conditions and more comorbidities, and a greater number of psychological problems such as severe anxiety, depression, and stress [7-9], all of which are associated with their long waiting times [9,10]. Moreover, these risk factors can negatively affect post-transplant outcomes. In particular, recent studies have reported that pre-transplant psychosocial factors can have a negative impact on post-transplant psychosocial status and on patient compliance with treatment regimens such as immunosuppressant medication [11], consequently adversely influencing transplantation outcomes, including mortality [12]. Therefore, a thorough pre-transplant psychosocial assessment of DDKT candidates is necessary during the waiting period to identify and address high psychosocial risk.
Current guidelines recommend a detailed evaluation of DDKT candidates, including their psychosocial characteristics [13]. Psychosocial assessment is an integral component of transplantation evaluation, especially because transplantation is a highly complex procedure that requires frequent pre- and post-transplant medical care and systematic management of the patient. Once listed as candidates, patients move into what may be the most stressful period of the entire transplantation process. Therefore, for an integrated and multi-dimensional psychosocial assessment, transplantation specialists and physicians should extend their evaluation beyond basic psychosocial health, to consider whether a candidate has strong social support, a suitable lifestyle for compliance with the treatment regimen, and a full understanding of the entire transplantation process [14]. However, little attention is given to the psychosocial status of DDKT candidates in Korea, who experience longer waiting times for transplantation than is the case in most Western countries.
Standardized screening tools and evaluation criteria are essential for successful DDKT candidate management in the clinical setting [14]. Although pre-transplant physical evaluation criteria are relatively well defined, pre-transplant psychosocial assessments are less standardized, and few evidence-based guidelines or universal criteria are available for them [13]. As a result, many different formal and informal psychosocial assessment methods are employed across transplantation centers. Furthermore, psychosocial assessments and systematic management of DDKT candidates by social workers or psychiatrists are not yet routinely performed at such centers, nor have they been integrated into the routine care of wait-listed patients [16]. The Psychosocial Assessment of Candidates for Transplantation (PACT) is a scale developed to assess factors influencing psychosocial outcomes in transplantation patients. It was originally created to support the clinical judgment of clinicians and has been used by transplantation team members to make decisions about patients’ candidacy [17]. The PACT is a validated instrument that assesses transplantation-specific psychosocial risk factors. It is a helpful and easy-to-use scale that any clinician completing a psychosocial assessment can use. Recent studies have employed standardized, transplantation- specific tools such as the PACT scale to assess whether pretransplant psychosocial risk predicted post-transplant mortality among liver and heart transplantation candidates [18,19].
Psychosocial status and risk factors have rarely been investigated among DDKT candidates. Although some studies have examined the pretransplant psychosocial status of transplantation candidates, only a few studies have addressed stress and coping [20], anxiety, or depression [21], examining single variables with a focus on psychopathology in such individuals, and those studies have not used a standardized, transplantation-specific tool to assess integrated psychosocial status and candidacy for kidney transplantation. Additionally, most of these studies focus on patients’ subjective experiences, conducted through self-report surveys. Therefore, these findings do not lead to prediction or management of vulnerable and high-risk patients in the clinical setting. Consequently, little reliable information is available about the psychosocial status of wait-listed candidates.
Therefore, the assessment of DDKT candidates’ psychosocial status using specific, standardized tools and the screening of their psychosocial vulnerability in the pretransplant period is of particular importance to allow transplantation teams to identify predictors of psychosocial risk.
2. Aims of the Study
The purpose of this study was to (1) assess the psychosocial status of DDKT candidates in Korea using the global PACT score, and (2) identify predictors of high psychosocial risk. The results of this study provide information on DDKT candidates’ psychosocial status that can guide transplantation teams in developing specific interventions for wait-listed candidates to enhance their psychosocial status and improve transplantation outcomes.
METHODS
1. Study Design
A descriptive, cross-sectional design was used for this study.
2. Participants
The study used a convenience sample of 157 DDKT candidates enrolled at an organ transplantation center (OTC) in Korea. Under the inclusion criteria, the study participants had to be 19 years of age or older, able to respond to the questionnaire, registered as a candidate in KONOS, and who had visited the OTC at least once to receive the 30-minute routine education from the kidney transplantation coordinator about guiding and preparing for DDKT.
Using the G*Power 3.1.9 program for statistical power analysis, the sample size was calculated to be 139, at a significance level of .05, a power of .80, and an effect size of .15 for logistic regression. Considering the expected attrition rate of 30%, 180 individuals were screened. The final sample consisted of 157 participants after excluding 23 individuals who failed to meet the inclusion criteria.
3. Data Collection
Data were collected from March 1 to December 31, 2017, through face-to-face interviews with participants using structured questionnaires, and from participants’ medical records and KONOS data. At the OTC, after a routine medical follow-up, eligible patients were asked by a researcher whether they were willing to participate in this study. The transplantation counseling room at the OTC was set as the data collection location to maintain patient comfort and confidentiality. For each participant, one interview, for an average of 30 minutes, was conducted to complete the psychosocial assessment.
The psychosocial assessment was performed by a KONOS-registered transplantation coordinator with over 10 years of work experience related to kidney transplantation. Each assessment included completion of the PACT scale, and utilized the information obtained from a comprehensive interview as well as from the social worker and nephrologist discussions with the participant. All KONOS-registered coordinators and nephrologists receive continuous training from transplant institutions in order to develop specialized care and communication skills for the management of patients. The coordinators in particular, play a unique role because they have the closest and most frequent contact with the patient. Prior to the psychosocial assessments, the coordinator and nephrologist received guidance from one of the original authors of PACT on how the instrument scores should be recorded. Finally, they agreed on each participant’s final PACT score, and after consultation with the participant, the nephrologist registered her/him as a candidate on the KONOS waiting list.
4. Ethical Considerations
This study was approved by the Institutional Review Board (IRB) of C University Hospital (IRB No. CUH 2015-07-008-002). The study’s purpose and procedures were explained to the patients and those who volunteered to participate provided written informed consent.
5. Measurements
1) Psychosocial Status
To assess participants’ psychosocial status, the PACT scale developed by Olbrisch, Levenson, and Hamer was used [17]. This tool consists of eight items, each having an initial rating and a final rating score. The eight items assess four characteristics of psychosocial significance: social support; psychological health; lifestyle factors, including compliance with medications; and understanding of transplantation and follow-up. Each item is rated on a five-point Likert scale ranging from 0 (poorest score) to 4 (best score). Higher ratings indicate greater appropriateness of candidates for transplantation. In the final assessment of a patient’s psychosocial risk, the evaluator integrates the ratings for all eight items into one final score: 0 for a poor candidate, 1 for a borderline candidate, 2 for an acceptable candidate, 3 for a good candidate, and 4 for an excellent candidate. A lower score indicates higher psychosocial risk.
The final score on PACT is not simply the summed total of the eight items because the instrument developers wanted to be able to weight factors that might be particularly significant for an individual patient. In accordance with the guidance manual prepared by the original authors of PACT, the eight initial scores for a participant were not equally weighted in arriving at a final rating [17]. For example, a participant may have scored well in all areas except one, but obtained a very low final rating due to the importance of that single area. Alternatively, other participants may have scored low due to an accumulation of minor problems in a number of areas. Ultimately, final ratings were assigned by referring to the initial ratings and to the PACT manual’s general descriptions of patients falling into each of the final rating categories.
The inter-rater reliability of the global PACT rating of candidates is 0.85 [17]. The criterion validity, explored by correlations between PACT and the Transplant Evaluation Rating Scale (TERS) in bone marrow transplantation patients, ranges from 0.68 to 0.89 [22]. Permission to use PACT in this study was obtained from the developers.
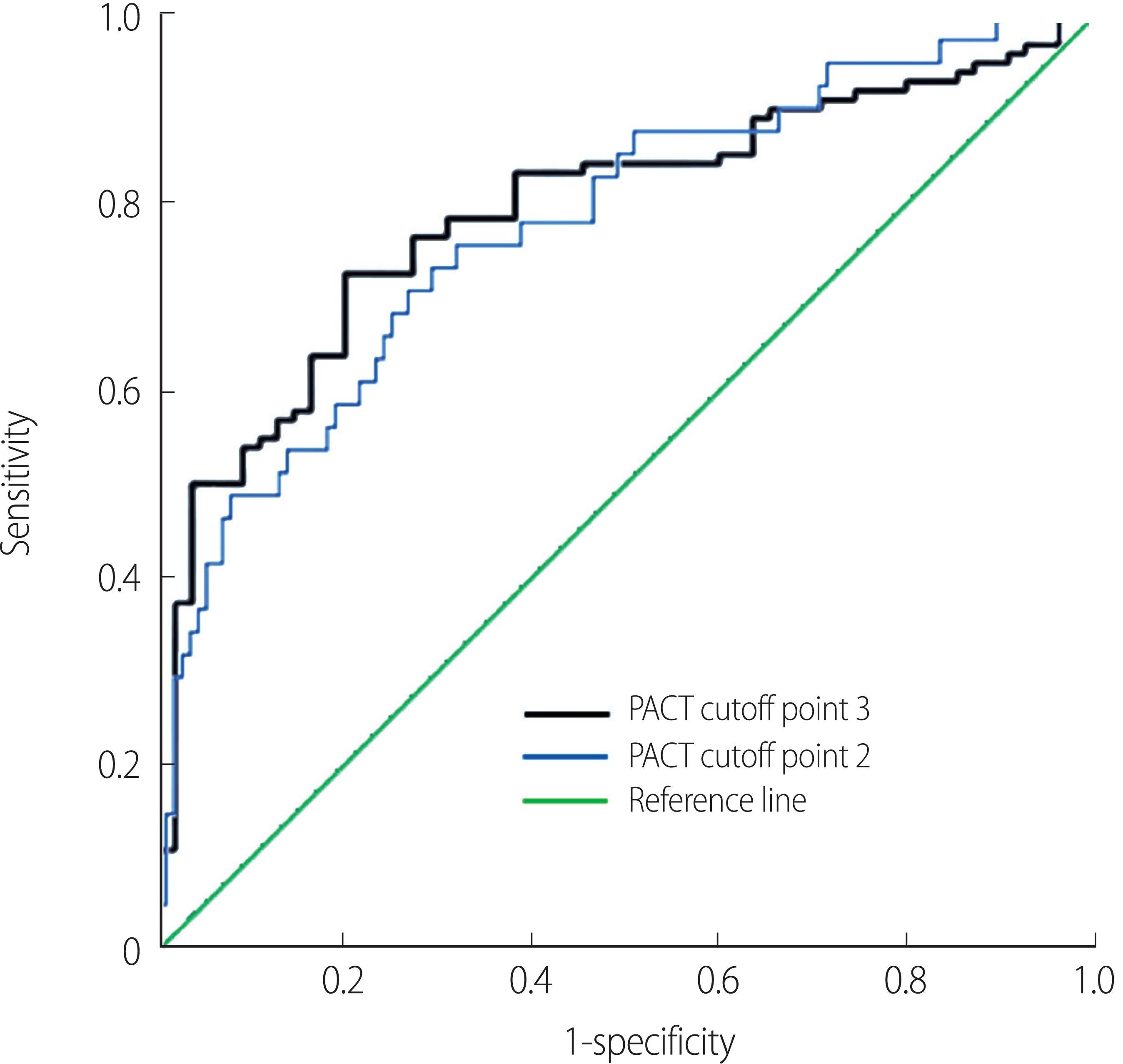
In this study, participants were divided into two groups: those having a PACT score <3 (poor, borderline, and acceptable candidates) were assigned to a high-psychosocial risk group, and participants with a PACT score ≥3 (good and excellent candidates) were placed in a low-psychosocial risk group. The cutoff value calculated the area under the curve (AUC).
2) Transplant-related Clinical Characteristics
Data were also collected on participants’ transplant-related clinical characteristics that might influence their psychosocial status. The clinical characteristics included body mass index (BMI), waiting time, location of dialysis, dialysis type and duration, panel reactive antibody (PRA) status, previous kidney transplantation, risk of a major cardiac event, and comorbidity.
Risk of a major cardiac event was assessed using the Revised Cardiac Risk Index (RCRI). RCRI is a useful tool for preoperative cardiovascular risk stratification in the kidney transplantation population undergoing noncardiac surgery. Each risk factor is entitled to one point; 0 points means the risk of a major CV incident is 0.4%, 1 point indicates the risk of CV incident is 0.9%, 2 points indicates a risk of 6.6%, and 3 or more points carry an 11% risk. RCRI scores were classified as indicating low or intermediate risk of major cardiac event (<3) or high risk (≥3).
Comorbidity was assessed using the Kidney Transplant Morbidity Index (KTMI), a transplantation-specific comorbidity index used to help determine physical candidacy by predicting the impacts of multiple pretransplant comorbid conditions on both graft and patient survival after transplantation. KTMI scores range from 0 to 11 and are assigned using a point-based scale. The total KTMI score reflects the patient’s age, years on dialysis, and BMI; the presence of diabetes, peripheral vascular disease, cerebral vascular disease, and coronary artery disease; previous transplantation; and functional status. KTMI scores ≥4 indicate that a patient is at high risk of graft failure or mortality [23].
3) Sociodemographic Characteristics
The sociodemographic characteristics assessed were age, gender, marital status, occupation, educational level, and type of health insurance.
6. Data Analyses
Psychosocial status and the sociodemographic and clinical characteristics were analyzed using descriptive statistics. Means and standard deviations were examined for continuous data, and frequencies and percentages were examined for categorical data. Binary logistic regression was performed to identify the potential predictors of psychosocial risk, which was a dichotomous variable. To determine predictors of high psychosocial risk, univariate logistic regressions were performed. The statistically significant variables in the univariate logistic regression analyses—KTMI score, RCRI score, waiting time, previous kidney transplantation, BMI, location of dialysis, age, gender, occupation, marital status, and type of health insurance—were included as covariates in a multivariate logistic regression by the enter procedure; the statistical significance level was set at p <0.05. Statistical analyses were conducted using SPSS version 22.0 (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corporation). For the PACT cutoff point test, the receiver operating characteristics (ROC) curve was used to analyze the test results in order to calculate the area under the curve (AUC) and a cutoff point for Korean DDKT candidates.
RESULTS
1. Participant Psychosocial Status
As shown in Table 1, the mean score of the PACT final rating was 2.10. Among the PACT subscales, participants’ social support was rated the highest (3.59), whereas understanding of the transplantation process and follow-up was rated the lowest (2.37).
2. Participant Demographic and Transplant-related Clinical Characteristics
Table 2 presents the demographic and transplant-related clinical characteristics of the study participants. The average age of the participants was 52.6 years (range: 19 to 72), and 58.6% of them were male. Most participants were married, had less than high school education, had no job, and were covered by Korean Medicare.
Among the participants’ clinical characteristics, more than half had received hemodialysis (HD) in a dialysis clinic outside the OTC, and the average duration of dialysis was 7.72 years. With regard to transplant-related factors, the mean waiting time was 5.26 years, and most participants had been awaiting DDKT for 5 or more years, had negative PRA, and had not had a previous kidney transplant. The participants’ mean BMI was 23.62.
As to transplant-related physical candidacy, both the KTMI and RCRI scores of most participants were above the intermediate level and indicated intermediate- or high-risk physical candidacy. The mean KTMI score was 3.73, and the mean RCRI score was 2.01.
3. Predictors of High Psychosocial Risk
Table 3 shows the predictors of high psychosocial risk among the participants. The results showed that increased odds of high psychosocial risk were significantly associated with older age, female gender, not being married (“others” marital status), having a job, higher KTMI score, higher RCRI score, lower BMI (<18.5 kg/m2), shorter waiting time (<5 years), receiving dialysis outside the transplantation center, and previous kidney transplantation.
When entered into a multivariate logistic regression model, two factors remained independently associated with high psychosocial risk; higher KTMI score (OR=8.62, p=.003) and older age (OR=7.37, p=.007) (Table 3). The likelihood ratio test of the binary logistic regression model indicated the statistical significance of the model with the covariates used (χ2=39.15, df=10, p<.001). In multivariate logistic regression analysis using three cut-off points, the classification accuracy, which indicates prediction accuracy of the model, was 76.4%. Therefore, the goodness of fit test was found to be suitable for the model.
4. ROC Curve Analysis of PACT Cutoff Points
As shown in Figure 1, the ROC curve analysis demonstrated the predictive power of PACT scores at different cutoff points: 2 and 3. The results of the ROC curve analysis were used to calculate the optimal PACT cutoff point indicating psychosocial risk for the Korean DDKT candidates. Specifically, when the AUC as a measure of predictive power was compared between the cutoff points of 3 and 2, the AUC of cutoff point 3 was higher (AUC=0.80; 95% CI=0.72-0.86) than that of cutoff point 2 (AUC=0.78; 95% CI=0.69-0.85). Thus, a PACT score of 3 as a cutoff point had greater predictive value for psychosocial risk among the Korean DDKT candidates and showed good discrimination as its AUC exceeded the 0.70 standard.
DISCUSSION
This study is meaningful in that it is the first performed in Korea to identify the psychosocial status levels of DDKT candidates by using a transplantation-specific measurement tool and examining related risk factors. Furthermore, the study findings indicate that PACT is a suitable tool for screening high-risk psychosocial status candidates, and a cutoff point for its application in the Korean clinical setting is proposed.
The present study revealed that the psychosocial status of the participants was susceptible level, as the final PACT mean score was 2.10. The study result was less than desirable, falling between the score of 2 indicating an “acceptable” candidate and the cutoff score of 3 indicating a “good” candidate. In comparison to other organ transplantation candidates, the mean participant score of 2.10 was lower than the 2.3 average among female liver transplantation candidates in the United States [18]; that is, the Korean DDKT candidates were somewhat vulnerable in terms of their psychosocial status. The results not only confirm previous research findings that psychosocial health such as depression and anxiety are vulnerabilities in candidates [24] but also show that being a candidate on a wait-list is in itself a less than ideal situation for the candidate’s psychosocial status. In other words, there is a possibility that the transplantation outcomes will be negative because the candidate is not well prepared in psychosocial terms before the transplantation procedure. Once patients are listed as candidates, they enter what may be the most stressful period of the entire transplantation process, especially because the candidates’ evaluation for transplantation suitability continues throughout their waiting period for a donated organ. In addition, given the recent issues associated with decreased organ donation in Korea, it is expected that the number of wait-list candidates who will experience longer waiting periods and thus increased psychosocial problems will increase in the short term. Therefore, there is an imperative need for a systematic management program for transplantation wait-list candidates that will not only support their psychosocial status but also enhance it to approach the ideal PACT score of 4.
Among the PACT subcategories, “understanding of the processes of transplant and follow up” showed the lowest score (2.30) in the study population. This finding was consistent with previous studies showing that candidates experienced psychological difficulties due to a lack of understanding of complex transplantation processes and expressed a high level of demand for improved process information and knowledge [25]. In particular, candidates’ understanding of important matters such as compliance with a follow-up regimen and requirements for providing annual blood samples for cross-matching is crucial, as inactivity in these regards can jeopardize their position on the wait-list under KONOS rules, and pose an increased risk of mortality. No systematic management programs currently exist for wait-list candidates to provide ongoing candidate education on these matters, as most OTCs offer only one-time education at the time of registration, and there is no standardized system for issuing blood sample reminders to candidates. Therefore, there is a clear need for transplantation teams to provide continuous education to candidates that recognizes their limited health literacy, a modifiable factor that is likely common among KT candidates [26].
In the present study, two factors—KTMI score and age—remained robust even after adjustment for other significant factors found in the bivariate analysis, including gender, marital status, employment status, previous KT, location and duration of dialysis, BMI, waiting time, and RCRI score. KTMI score and age may explain the high level of psychosocial risk in the study sample of DDKT candidates.
First, KTMI score was the strongest predictor of high psychosocial risk in this study. In other words, higher KT physical candidacy risk in candidates was significantly and independently associated with psychosocial status risk. A higher burden of pre-KT comorbidities has been associated with increased risk of post-KT mortality [27], and the present study found that comorbidity burden negatively affected candidates’ psychosocial status. Based on these findings, transplantation teams should continuously assess DDKT candidates’ psychosocial status and, particularly for those with higher KTMI scores, should implement interventions to improve their psychosocial status. Doing so on a continuous basis is crucial to ensure that candidates are ready for emergency transplantation surgery when a donor suffers brain death.
Second, older age was also a predictor of high psychosocial status risk in this study, indicating that older candidates are at greater psychosocial risk. Therefore, transplant coordinators and nurses should regard older candidates as a high-risk group and should closely monitor their psychosocial status; when necessary, interventions that focus on older candidates’ areas of PACT vulnerability should be provided. Especially because the average age of KT candidates is increasing and thus the number of elderly wait-list candidates is growing [5], a wait-list management strategy that is sensitive to candidate age is needed.
According to the results of the binary logistic regression, there was a significant association between waiting time up to 5 years for DDKT and high psychosocial risk. However, in the final multivariate logistic regression model, waiting time and other sociodemographic and clinical factors did not explain high psychosocial risk. This finding differed from the results of a previous study indicating that depression, anxiety, and longer waiting time were significantly related [28]. The present study included participants having a waiting period of up to 10 years, but the previous study’s subjects had been wait-listed for no more than 2 years. Therefore, further research is needed to more conclusively determine the association between waiting time and psychosocial risk. Because this is the first study to assess the psychosocial status of DDKT candidates using a transplantation-specific PACT tool, future researchers should give particular attention to the predictors found to be non-significant in this study.
For accurate application of any assessment tool, an appropriate cutoff is needed for each clinical setting. The original developers of the PACT did not recommend a cutoff point for the tool, leaving that determination to individual researchers. In this study’s comparison of PACT cutoff points of 2 and 3 through ROC analysis, the AUC was 0.80 when the cutoff was 3 points. The same cutoff value was used in previous studies that explored the relationship between the PACT final score and mortality in lung transplantation candidates [29] and pediatric kidney transplantation candidates [15]. Other studies that revealed relationships between the PACT final score and mortality in liver and lung transplantation candidates used cutoffs of 2 and 3, respectively [18,30]. These differences in the selection of cutoff points are thought to be attributable to regional and cultural differences in the study samples. In the present study, a cutoff point of 3 on PACT was determined to be suitable to screen the patient population for high psychosocial risk in the Korean clinical context.
Limitations of this study include its cross-sectional design and recruitment from a single Korean OTC, which may reduce the generalizability of its findings. Nevertheless, this research provides new and crucial information that can help clinical nurses and other transplantation specialists to implement interventions for improving the psychosocial status of DDKT candidates. Recommendations for further research include using samples of DDKT candidates recruited from multiple OTCs and intensifying efforts to develop standardized tools to measure the psychosocial status of Korean wait-listed candidates.
CONCLUSION
The psychosocial status of the Korean DDKT candidates in this study was found to be less than ideal, and their poor understanding of the transplantation process made them especially vulnerable. Poor physical candidacy for DDKT, particularly due to the presence of comorbidities, and older age were associated with high psychosocial risk. Both clinical strategies and intervention programs are needed to enhance psychosocial status among Korean DDKT candidates. Transplantation teams can use the information from this study and appropriate tools to screen patients with high-risk psychosocial status early in the transplantation process and can provide intensive interventions to enhance psychosocial status, particularly for those with poor physical candidacy and older candidates.
CONFLICT OF INTEREST
The author declared no conflict of interest.