Adherence to antiretroviral therapy and associated factors among HIV-positive adolescents in Sub-Saharan Africa: a systematic review
Article information
Abstract
Purpose
Although long-term viral suppression and antiretroviral therapy (ART) success depend on sustained adherence, adolescents’ adherence rates are suboptimal. Optimal adherence is influenced by various factors. Since Sub-Saharan Africa is home to over 80% of adolescents living with human immunodeficiency virus (HIV) and considering their unique characteristics and susceptibility to poor adherence, it is crucial to provide updated knowledge on adherence rates and their determinants among this population. This review aims to present up-to-date data on adherence rates and associated factors among HIV-positive adolescents in Sub-Saharan Africa.
Methods
A systematic review was conducted following the PRISMA guidelines. The PubMed and Scopus databases were used to identify documents corresponding to the study's objectives. Eleven studies were included in this review after being selected from among all studies that were found online from 2017 to 2023.
Results
The reported adherence rates ranged from 55% to 86%. In total, 32 factors were found to be related to adherence among HIV-positive adolescents in Sub-Saharan Africa. These included 12 adherence-facilitating factors and 20 adherence-inhibiting factors. The most often mentioned factors affecting adherence were advanced World Health Organization clinical stage (i.e., stage IV), ART dose and regimens, a lack of support, and violence victimization.
Conclusion
Our findings can help healthcare providers collaborate with HIV-positive adolescents to improve ART adherence and ensure the best possible health outcomes.
INTRODUCTION
Human immunodeficiency virus (HIV) continues to be a major global public health problem with approximately 38.4 million people living with HIV at the end of 2021 with 1.5 million new infections and 650,000 AIDS-related deaths globally [1]. In Africa, 25.6 million people were living with HIV and an estimated 880,000 new infections and 460,000 deaths were attributed to HIV related in 2020 [2,3].
Adolescence is the period of life between childhood and adulthood, from 10 to 19 years [4]. Given their rapid physical, psychological, and physiological changes, which have an impact on their health-related behaviors, adolescents are a particularly vulnerable age group when it comes to acquisition of HIV infection [5]. In the world at the end of 2021, there were about 1.8 million adolescents who were HIV positive, with more than 1.5 million of them residing in Sub-Saharan Africa [2,3,6,7]. The long-term survival of perinatally infected children and newly infected adolescents globally has led to a growing number of people living with HIV in this age group, with the highest proportion residing in the Southern and Eastern regions of Africa [8,9].
Antiretroviral therapy (ART) has significantly reduced AIDS-related morbidity and mortality in general population worldwide [10]. The goal of ART is to reduce viral replication, protecting HIV-positive individuals from AIDS-related diseases and death as well as stopping further virus transmission [11,12]. However, adolescents are the only age group in which AIDS-related deaths are not decreasing [13]. In Eastern and Southern Africa, AIDS-related deaths among adolescents have been increased in the last decade [14].
For the success of ART, treatment adherence plays an important role. Treatment adherence is defined as the extent to which a person’s behavior of taking medication, following a diet, and/or executing lifestyle changes, corresponds to agreed recommendations from a healthcare provider [15,16]. Adolescents and children who are HIV-positive and receiving ART show poorer treatment adherence and lower rate of viral suppression compared to adults [17]. Adolescents are not only a vulnerable population to the HIV infection but also to the disease progression associated with poor adherence [18]. Especially, adolescents living with HIV have a higher likelihood of suboptimal adherence, viral replication, loss-to-follow-up, morbidity, and mortality [14,19].
Poor adherence results in inadequate drug exposure and increases the likelihood of viral replication and resistance, which might limit future therapeutic options and leading to disease progression and increases onward transmissions [10,19,20]. In addition, sometimes adolescents are neglected in the planning of healthcare services as a result they might disappointed and lost to follow-up [10]. Thus, it is important to update the knowledge regarding ART adherence and associated determinants among adolescents because Sub-Saharan Africa is home to more than 80% of adolescents living with HIV [21] and because of their unique nature and vulnerability to suboptimal adherence.
Therefore, this systematic review was done to present up-to-date data on the adherence rate and related factors among adolescents living with HIV in Sub-Saharan Africa.
METHODS
A systematic review of peer-reviewed articles published on journals about antiretroviral therapy adherence and associated factors among HIV-positive adolescents in Sub-Saharan Africa was performed from December 1, 2022 to February 13, 2023. A systematic review was conducted by following the updated reporting guideline or checklist of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Search strategy
The potential articles were obtained online from database including PubMed, and Scopus using the combination of keywords and Boolean operators (AND, OR, NOT). A comprehensive search of articles was performed by utilizing adolescent, HIV, antiretroviral adherence, art adherence and art compliance as keywords to find the articles contained these words in their titles or abstracts.
PubMed searching terms were resulted a total of 209 studies. Scopus searching terms were “TITLE-ABS-KEY ( adolescent* AND hiv AND art AND adherence OR antiretroviral AND adherence OR art AND compliance ) AND ( LIMIT-TO ( OA , "all" ) ) AND ( LIMIT-TO ( PUBYEAR , 2022 ) OR LIMIT-TO ( PUBYEAR , 2021 ) OR LIMIT-TO ( PUBYEAR , 2020 ) OR LIMIT-TO ( PUBYEAR , 2019 ) OR LIMIT-TO ( PUBYEAR , 2018 ) OR LIMIT-TO ( PUBYEAR , 2017 ) ) AND ( LIMIT-TO ( DOCTYPE , "ar" ) ) AND ( LIMIT-TO ( SUBJAREA , "MEDI" ) OR LIMIT-TO ( SUBJAREA , "IMMU" ) OR LIMIT-TO ( SUBJAREA , "PSYC" ) OR LIMIT-TO ( SUBJAREA , "PHAR" ) OR LIMIT-TO ( SUBJAREA , "NURS" ) ) AND ( LIMIT-TO ( EXACTKEYWORD , "Adolescent" ) ) AND ( LIMIT-TO ( SRCTYPE , "j" ) )” yielded out 350 articles.
We had utilized search filters and limits like adolescent, open access, abstract, journal articles, area (medicine, immunology, psychology, nursing, sociology, and pharmacology), and studies conducted and published 2017 to 2022. We included studies conducted in 2017 and after because World Health Organization (WHO) updated and launched new policy recommendations on the clinical and service delivery aspects of HIV treatment and care in late 2016 [22].
Eligibility criteria
Inclusion criteria: the studies fulfilling these criteria were included in a systematic review. 1) Study participants: adolescents (10 to 19 years); 2) reported study outcomes: adherence rate or associated factors; 3) design: quantitative, qualitative, or mixed; 4) peer-reviewed articles; 5) studies conducted in Sub-Saharan African countries.
Exclusion criteria: those studies included pediatric age group <10 years or adults, studies not reported adherence rate or associated factors or reported other outcomes were excluded.
Selection and data extraction processes
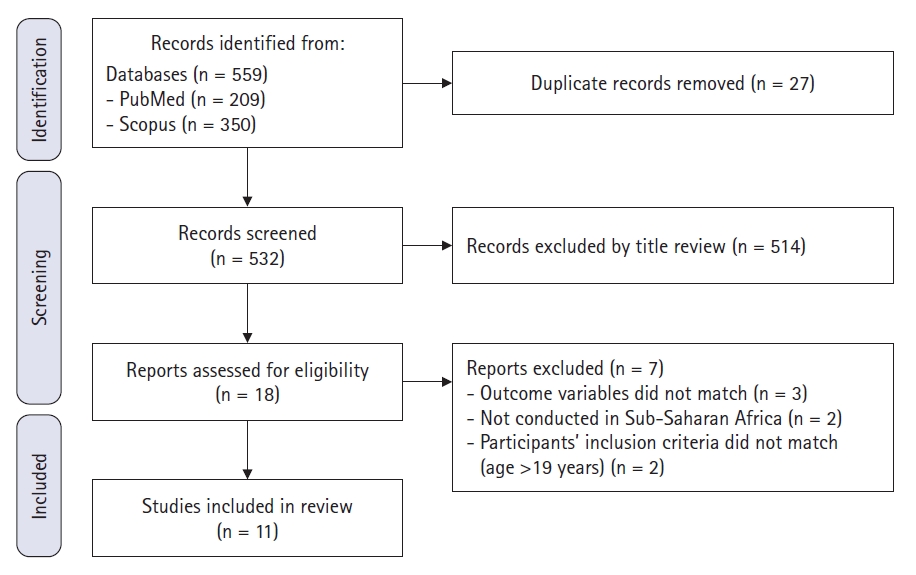
After searching for potentially eligible studies from the databases, the titles, abstracts, authors’ name, and publication years of the articles were exported to EndNote 20 reference manager for further processing. The duplications were checked and removed using EndNote’s find duplication. Subsequently, the titles, abstracts and full texts screening were performed by two investigators independently and potentially eligible studies were selected for final review. Before the final decision for review, the quality of each article was assessed using critical appraisal tools and checklists: Newcastle-Ottawa-Scale (NOS) [23] for quantitative studies. As a qualitative study’s validity is reliant on the statement of the question, theoretical or conceptual framework, design, method, sample, and data analysis [24], the two authors independently conducted a thorough review and critique of the three qualitative studies [25-27]. Each author evaluated them independently and brought out their evaluations of the papers to the table for discussion. Following discussion, we agreed to include the three studies. The two authors independently examined the extracted data, and any disagreements in the extracted data were deliberated and resolved. The extracted data was summarized and reported in table and text form. The associated factors were grouped as facilitators and inhibiting factors of antiretroviral adherence. Primary electronic data searching was yielded out 559 studies (Figure 1).
Ethical considerations
This study received exempt review approval form the Institutional Review Board of Keimyung University (IRB No. 40525-202308-HR-042-01) due to the anonymous nature of the survey and absence of sensitive information.
RESULTS
Selection process
The initial search through databases yielded a total of 559 studies. Then duplicate was checked using EndNote, and 27 articles were removed. The remaining studies were screened through title reading, and 514 studies were excluded. Eighteen studies screened through abstract and full-text review, and finally 11 articles were included in this systematic review (Figure 1).
Characteristics of included studies
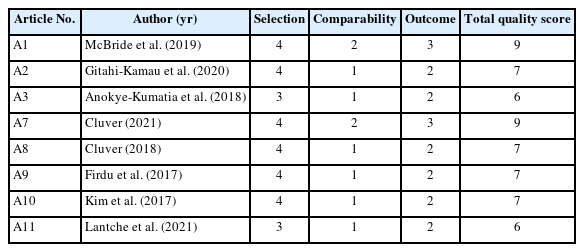
All the included studies conducted on the total sample of 10,297 participants. The included studies conducted in eight Sab-Saharan African countries from Eastern, Southern and Western regions from 2017 to 2022. Two studies were cohort design (one prospective and one retrospective), six studies were cross-sectional design, two studies were mixed, and one study was qualitative design (Table 1). The quality assessment for each quantitative study performed using NOS (Table 2).
Adherence rate and measurements
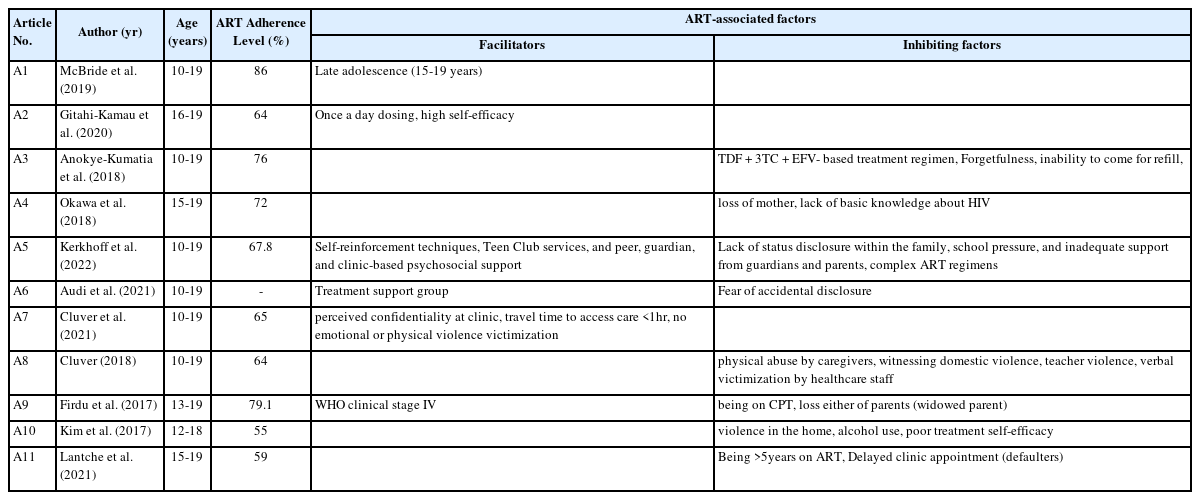
All included studies reported the treatment adherence rates, except for the one qualitative study [27]. The overall reported adherence rate ranged from 55% to 86%. Regarding the ART adherence measure, eight of the studies employed self-reported methods [25, 28-34], and two studies measured using pill count techniques [26,35] .
Factors affecting treatment adherence
Of the eleven studies reviewed, ten studies reported both the adherence rates and associated factors as their primary outcomes. But the remaining study reported only associated factors as its primary outcome (Table 3). Three studies reported both facilitators and inhibiting factors [26, 27, 31] while five studies revealed only inhibiting factors [25,29,32-34], and the remaining studies reported only enhancing factors [28,30,35].
This review identified a total of 32 factors associated with antiretroviral adherence among the study participants in Sub-Saharan Africa (Table 3). Twelve factors were identified as facilitating, and twenty as inhibiting. The facilitating factors include sociodemographic factors (age), treatment skills (high treatment self-efficacy, and self-reinforcement techniques), advanced disease stage (WHO clinical stages IV), psychosocial support (support from peers, guardians, teen clubs, and treatment support groups, perceived confidentiality at clinic, absence of violence and abuse), treatment-related factors (simplified dosages, and short travel time to get access to healthcare). On the other hand, inhibiting factors include treatment-related factors (ART regimen complexity and side-effects, and burden from cotrimoxazole preventive therapy, inability to come to the clinic for refill, and delayed clinic appointment), violence and abuse (at home by caregivers, at school by teachers, and at healthcare clinics by healthcare providers), cognitive and memory associated factors (lack of basic knowledge about HIV, forgetfulness), lack of support (loss of either parent, inadequate support from guardians and parents), disclosure issues (lack of status disclosure within the family, fear of accidental disclosure), poor treatment self-efficacy, alcohol use, and long-term on ART.
DISCUSSION
The studies included in this review were, the studies conducted among HIV-positive adolescents and reported adherence rates or associated factors as a primary outcome. In this review, the adherence rate ranged from 55% to 86%. This adherence rate is substantially below optimal adherence, which is vital for viral load suppression and the prevention of further transmissions. Kim et al. [33] and Lantche et al. [32] revealed a considerably lower adherence rate than other studies included in the systematic review. This variation may be attributed to differences in healthcare systems across countries, as well as the diverse methods employed within individual studies. For instance, the research carried out in Malawi by Kim et al. [33] and Villiera et al. [26] employed distinctly different methods, potentially leading to varied findings. Moreover, the disparity in findings might be due to the various adherence measurement techniques. Kim et al. [33] reported adherence over the past 30 days, whereas Lantche et al. [32] utilized a combination of quantitative, qualitative, and mixed methods for self-reported adherence. Constant adherence is essential for immune system stability, virologic suppression, and the avoidance of opportunistic infections [36].
Adherence to ART treatment was more common in older adolescents. The late adolescence stage is when adolescents are more mature and start taking responsibility for their health, hence it may be related to their developmental stage [35]. HIV infection is classified according to its clinical stage by WHO, with Stage III and Stage IV indicating severe phases of the illness. Adolescents with an advanced stage of the illness may be more likely to take their medications as prescribed. This may be related to the fear of a more serious illness and more serious health consequences if they don't take their medication consistently. The studies have reported that an advanced WHO clinical stage is associated with improved adherence in adolescents [31,37].
Adherence to ART may be challenging for adolescents with HIV due to the difficulties they confront. These difficulties could include stigma, social exclusion, a lack of support from peers and family members, and the stress of managing a complex treatment regimens. Self-efficacy can help to reduce some of these difficulties by giving adolescents the confidence and motivation they need to follow their treatment. Adolescents with high levels of self-efficacy were more likely to adhere to their treatment plan [38,39]. Thus, self-efficacy-focused interventions can increase adherence rates in adolescents, which will ultimately lead to better health outcomes.
ART adherence among adolescents can be affected by the complexity of drug regimen and the side-effects of the medications. If many pills must be taken at various times throughout the day, adolescents may find it more challenging to continuously remember to take their medication. In addition, adolescents may be more prone to forgetting or skipping dosages if they are experiencing side effects [26,29,37,40]. Using fixed-dose combinations or single dose per day which can simplify drug regimen complexity and adjust the medication regimen as needed can help to improve adherence among adolescents.
Adolescents may also be more likely to follow their ART treatment if they have strong psychosocial support and a positive relationship with their healthcare provider [41]. Support and reminders from family or caregiver and peers, as well as friendly communication and understanding with their healthcare provider, can improve adolescents’ knowledge and confidence about their treatment which contribute to better adherence [10]. Adolescent peer support groups can be especially beneficial for adolescents, as they may be more likely to rely on their peers for advice and guidance due to their unique characteristics [27]. In this group adolescents living with HIV can share their feelings with others who are going through similar experiences, which can help them feel less alone and more motivated to adhere to their ART treatment.
Adolescents' adherence to ART might be significantly impacted by violence and abuse since these conditions can make it more difficult for them to remember to take their medication regularly. Adolescents who live in violent homes, experience violence at school, and feel intimidated or insecure while they are in a healthcare setting may not be able to access medication or be afraid to take it. They may also be less inclined to attend clinic sessions [34]. Therefore, to prevent any forms of abuse and violence, it is crucial to collaborate with family, caregivers, teachers, and healthcare professionals.
Lack of disclosure within the family and fear unintended disclosure may have a negative influence on adolescents' adherence to ART. If the adolescents reveal their HIV status to others, they might experience stigma and discrimination. However, adolescents living with HIV who disclose their status to family members and supportive peers may be more likely to take part in peer support groups and have social support, which might encourage them to take their medication constantly [26,27]. Thus, more research is needed to determine the most secure method of telling close friends and family members about their HIV status.
In general, it's critical to uncover any factors that may have an impact on adolescents ART adherence. This enables healthcare professionals to collaborate better with adolescents to improve ART adherence and guarantee the best possible health outcomes. One of the limitations of this systematic review is publication bias as it included only the articles published on journals. In addition, in consideration of the investigators’ language ability, the reviewed articles were limited to those articles published in English.
CONCLUSION
This systematic review included updated information on ART adherence rates and associated factors among HIV-positive adolescents in Sub-Saharan Africa, as reported in published articles. A total of 32 factors associated with ART adherence among adolescents in the region were found in the assessment of articles from 8 Sub-Saharan Africa countries. These factors include age, forgetfulness, advanced WHO clinical stages, ART dosing, side-effects and drug regimens, psychosocial support, treatment self-efficacy, lack of support, violence victimization, confidentiality concerns, disclosure issue, long-term on ART, delayed clinic appointments and travel time to access ART services.
Notes
CONFLICT OF INTEREST
Sangeun Jun has been an editorial board member of the JKBNS since 2018. However, she was not involved in the review process of this manuscript. Otherwise, there was no conflict of interest.
AUTHORSHIP
GGG and SJ contributed to the conception and design of this study; GGG collected data; GGG and SJ performed the statistical analysis and interpretation; GGG and SJ drafted the manuscript; GGG and SJ critically revised the manuscript; SJ supervised the whole study process. All authors read and approved the final manuscript.
FUNDING
None.
DATA AVAILABILITY
Please contact the corresponding author for data availability.
References
Appendices
Appendix 1. List of articles included in this review
1. McBride K, Parent J, Mmanga K, Chivwala M, Nyirenda MH, Schooley A, et al. ART adherence among Malawian youth enrolled in teen clubs: a retrospective chart review. AIDS and Behavior. 2019;23(9):2629-33. https://doi.org/10.1007/s10461-019-02580-y
2. Gitahi-Kamau N, Wahome S, Bukusi EA, Ngure K. Determinants of antiretroviral therapy adherence among older adolescents living with HIV in Kenya during the transition to adult care; an observational study. Journal of AIDS and HIV Research. 2020;12(2):24-33. https://doi.org/10.5897/jahr2020.0513
3. Anokye-Kumatia AB, Enimil A, Afriyie DK, Tetteh R, Mensah NK, Amo AA, et al. Highly active antiretroviral therapy adherence among perinatally infected HIV adolescents at a teaching hospital in Ghana. AIDS Care. 2018;30(9):1144-1146. https://doi.org/10.1080/09540121.2018.1494263
4. Okawa S, Mwanza Kabaghe S, Mwiya M, Kikuchi K, Jimba M, Kankasa C, Ishikawa N. Psychological well-being and adherence to antiretroviral therapy among adolescents living with HIV in Zambia. AIDS Care. 2018;30(5):634-642. https://doi.org/10.1080/09540121.2018.1425364
5. Villiera JB, Katsabola H, Bvumbwe M, Mhango J, Khosa J, Silverstein A, et al. Factors associated with antiretroviral therapy adherence among adolescents living with HIV in the era of isoniazid preventive therapy as part of HIV care. PLOS Global Public Health. 2022;2(6). https://doi.org/10.1371/journal.pgph.0000418
6. Audi C, Jahanpour O, Antelman G, Guay L, Rutaihwa M, van de Ven R, et al. Facilitators and barriers to antiretroviral therapy adherence among HIV-positive adolescents living in Tanzania. BMC Public Health. 2021;21(1):2274. https://doi.org/10.1186/s12889-021-12323-1
7. Cluver L, Shenderovich Y, Toska E, Rudgard WE, Zhou S, Orkin M, et al. Clinic and care: associations with adolescent antiretroviral therapy adherence in a prospective cohort in South Africa. AIDS. 2021;35(8):1263-71. https://doi.org/10.1097/qad.0000000000002882
8. Cluver L, Meinck F, Toska E, Orkin FM, Hodes R, Sherr L. Multitype violence exposures and adolescent antiretroviral nonadherence in South Africa. AIDS. 2018;32(8):975-983. https://doi.org/10.1097/QAD.0000000000001795
9. Firdu N, Enquselassie F, Jerene D. HIV-infected adolescents have low adherence to antiretroviral therapy: a cross-sectional study in Addis Ababa, Ethiopia. Pan African Medical Journal. 2017;27:80. https://doi.org/10.11604/pamj.2017.27.80.8544
10. Kim MH, Mazenga AC, Yu X, Ahmed S, Paul ME, Kazembe PN, Abrams EJ. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. Journal of the International AIDS Society. 2017;20:21437. https://doi.org/10.7448/IAS.20.1.21437
11.Lantche MW, Fokam J, Cheudjui AJN, Tchatchueng JBM, Noumsi TSJ, Ateba FN, et al. Factors associated with non-adherence to antiretroviral therapy among HIV-infected adolescents aged 15-19 years: a snapshot from the mother and child center in Yaounde, Cameroon. Pan African Medical Journal. 2021;39:154. https://doi.org/10.11604/pamj.2021.39.154.27623